






The Tower Hamlets Civic Awards recognise individuals who live, work, or study in the area and help improve the quality of life for others. The awards celebrate outstanding service to the community, achievements in sports, arts, or culture, contributions that enhance the quality of life beyond paid duties, and success in business combined with community involvement.
Nominated by the Centre for Public Engagement and Civic team at Queen Mary, Dr Kathleen McCarthy (School of the Arts) and Professor Alastair Noyce (Wolfson Institute of Population Health) were recognised for their work in improving the quality of life for local people and Dr Sara Paparini (Wolfson Institute of Population Health) was recognised for community involvement in research.
Dr McCarthy, Professor Noyce and Dr Paparini lead work that makes a significant contribution to Queen Mary’s civic work in, with and for east London and the priority themes on ‘healthy and sustainable futures’ and ‘pathways for life’ in our Civic University Agreement. Their work with Tower Hamlets Education Partnership, Osmani Trust and Positive East features in three films on Queen Mary’s research partnerships with voluntary and community sector organisations in east London.
Dr Sara Paparini is the social science lead for the SHARE Collaborative and leads the ‘Partnership for Black People’s Health’ project, engaging Black African and Black Caribbean communities in co-produced research to mitigate health disparities. Her work with the ‘Harnessing Collective Power’ initiative, commissioned by Tower Hamlets Council, amplifies community voices in local policymaking, empowering residents to participate in research and policy development.
The awards ceremony took place 23 April in Mile End Park’s Ecology Pavilion. In the presence of distinguished guests and leaders from local organisations and government, award winners were celebrated for their service to Tower Hamlets. It was truly remarkable to see the breadth of recipients’ commitment to their local community, from improving people’s health, supporting children and young people, and investing in education and local infrastructure.
Dr Philippa Lloyd (Vice-Principal Policy and Strategic Partnerships) and Professor Alison Blunt (Deputy Vice-Principal for Impact [Culture, Civic and Community]) have congratulated the Queen Mary academics for their recognition – “Many congratulations to Alastair, Kathleen and Sara on receiving Tower Hamlets Civic Awards. The awards recognise their outstanding work with local partners and communities on health and education, both key priorities for Queen Mary’s civic and community engagement in Tower Hamlets and across east London”.

Below is a short film made by the QMUL CPE team showcasing the work the SHARE collaborative does in partnership with Positive East (a voluntary sector organisation), as well as other types of community engagement we are actively involved in. Please take some time to check this video out.
Thank you to Tower Hamlets for hosting this award ceremony and for honouring the amazing work Dr Paparini is involved in at the SHARE collaborative. For further information on the remaining categories and the work Dr McCarthy and Professor Noyce were awarded for, please follow this link.
Beyond the Clinic is a new study from the SHARE collaborative exploring the potential for equitable implementation of long-acting injectable cabotegravir for PrEP outside of sexual health clinics among PrEP providers and potential PrEP providers in the UK.
Pre-exposure prophylaxis (PrEP) is a highly effective medication that HIV-negative people can take before and after sex to reduce their risk of getting HIV.
Until now, PrEP has only been available in the UK as a pill, taken daily or before and after sex. However, long-acting injectable cabotegravir (CAB) for PrEP has very recently been approved for NHS provision in Scotland and is currently undergoing assessment for provision in England and Wales.

CAB for PrEP is an intramuscular injection taken once every two months. It has been shown to be very effective at preventing HIV as people find it easier to adhere to than taking oral pills every day. People may also prefer CAB for PrEP as it is more discreet than carrying pills. Women have especially been found to prefer CAB for PrEP over pills.
Currently PrEP is only available from NHS sexual health clinics in the UK. However, some people may find it difficult to access PrEP because of the stigma associated with using sexual health services and this can increase health inequities.
Women, heterosexual men, racially minoritised communities, trans and gender diverse people and young people are less likely to take PrEP. Making PrEP, including CAB for PrEP, available in other settings outside of sexual health clinics (such as pharmacies, GP practices and third sector organisations) could make accessing PrEP easier for them.
If you work in a sexual health clinic and would like to sign up to be notified of the survey launch in June, please sign up here.
We want to understand what current and potential PrEP providers think about the feasibility of delivering CAB for PrEP in clinics and in alternative settings, such as pharmacies, GP practices and drug and alcohol services. This will include exploring what the barriers are to implementing PrEP beyond the sexual health clinic.
We also want to understand how they think this might improve equitable access to PrEP, including CAB for PrEP.
The information we gather will help us to develop recommendations on ways to optimise implementation of CAB for PrEP so that PrEP uptake and use is more equitable across all the groups who may benefit from it.
We will share our recommendations with policymakers, commissioners and service providers with the hope of influencing how CAB for PrEP is delivered in the UK.
The Beyond the Clinic study has three phases. Each study phase will be informed by the previous one.
First, interviews with current PrEP providers (i.e. sexual health clinicians) will help us to understand the topic in more depth and identify the best survey questions to ask sexual health clinicians about implementing CAB for PrEP beyond the clinic.
Second, a brief survey will be sent to all sexual health clinics in the UK to understand the breadth and scale of the issues which may impact equitable implementation of CAB for PrEP beyond the clinic in the UK.
Third, interviews will be conducted with potential PrEP providers in alternative settings, such as pharmacists, drug and alcohol service providers and GPs, to understand the issues from their perspective.
The Principal Investigator for the study is Dr Sara Paparini. The other study team members are Prof Chloe Orkin, Dr Melanie Smuk, Rosalie Hayes and Nishat Halim.
SHARE has a paid community advisory board of people living with HIV who provide strategic oversight and guidance on all our studies.
In addition, the Beyond the Clinic study has an Expert Advisory Group whose will provide advice and guidance to the study team. Our EAG members are:
This study is being funded by ViiV Healthcare.
For any questions about the study, contact beyondtheclinic@qmul.ac.uk. Follow our social media accounts for regular updates about the study.

The awards ceremony, held on 12th Sept 2024 at the Royal College of Physicians in London, brought together nominators, nominees and their team members to recognise exceptional work and expertise delivered by teams and individuals from across the 23 Trusts within the CRN NT remit. This was the first time such an ceremony has been hosted by the CRN NT.
The ILANA Team found success during this ceremony by securing two nominations in two different categories, one for Innovative in Reducing Health Inequalities and the second being Excellence in PPIE.
The ILANA Team successfully won the category for Innovation in Reducing Health Inequalities. This is due to the groundbreaking work the team conducted in promoting an anti-sexist, anti-ageist and anti-racist study design.

The Award for Innovation in Reducing Health Inequalities

Our ILANA Trial Manager, Nishat Halim and Programme Manager, Sadna Ullah who represented the whole ILANA Team at the ceremony
Thank you to CRN NT for hosting this award ceremony and for honouring us with an amazing award. For further information on the remaining categories and other awards won, please follow the link here.
Farooq HZ, Whitton L, Mwendera C, Divall P, Spitters S, Anderson J, Thornhill J. Virtual care pathways for people living with HIV: A mixed-methods systematic review. HIV Med. 2024; 1–26. doi:10.1111/hiv.13701
Abstract
The COVID-19 pandemic prompted an unprecedented surge in virtual services, necessitating a rapid shift to digital healthcare approaches. This review focuses on evaluating the evidence of virtual care (VC) in delivering HIV care, considering the complex nature of HIV and the need for tailored-approaches, especially for marginalized populations.
A mixed-methods systematic review was performed with searches on five databases, covering studies from January 1946 to May 2022. Inclusion criteria involved two-way virtual consultations between healthcare workers and people living with HIV (PLHIV), with detailed descriptions and outcomes. Qualitative and quantitative studies were included, and the risk of bias was assessed using the Newcastle–Ottawa score and Stenfors’ framework.
Among 4143 identified records, 26 studies met the criteria, with various models of care described. The majority of studies were observational, and videoconferencing was the primary mode of virtual consultation employed. Quantitative analysis revealed PLHIV generally accept VC, with high attendance rates (87%). Mean acceptability and satisfaction rates were 80% and 85%, respectively, while 87% achieved HIV viral suppression. The setting and models of VC implementation varied, with some introduced in response to COVID-19 while others were as part of trials.
VC for PLHIV is deemed an acceptable and effective approach and is associated with good virological outcomes. Data on other health outcomes is lacking. The review underscores the importance of diverse models of care, patient choice and comprehensive training initiatives for both staff and patients. Establishing a ‘gold standard’ for VC models is crucial for ensuring appropriate and effective reviews of PLHIV in virtual settings.
The announcement of Professor Orkin’s MBE recognises her outstanding achievements as a world-leading HIV researcher, clinician, and medical, LGBTQ+ and disability leader.
The announcement of Chloe’s MBE falls in Pride Month, and there’s no better occasion to recognise Chloe’s fantastic achievements to medicine and equality, as well as her role as a prominent clinician activist leader for HIV communities and a medical, LGBTQ+ and disability leader.
Chloe Orkin (Director of the SHARE Research Collaborative) is Professor of Infection and Inequities at Queen Mary and a Consultant Physician at Barts Health NHS Trust.
Chloe’s pioneering research led to the licensing and implementation of the first-ever injectable treatment for HIV. The treatment improves the quality of life for people living with HIV – for the first time, people living with HIV could choose to receive treatment through an injection every two months, rather than take daily pills. You can learn more about the research SHARE conduct here.
While Chair of the British HIV Association in 2017, she spearheaded the UK arm of the ‘Undetectable = Untransmissible’ (U=U) campaign, which highlighted that there is zero risk of HIV transmission for people taking effective antiretroviral treatment. The global campaign has been transformative in reducing stigma for people living with HIV.
Her ground-breaking research on the clinical features of mpox has shaped our understanding of the condition, and her work has set new standards and guidelines in the treatment of these conditions.
Orkin is equally committed to equity for healthcare professionals. She was the first LGBTQ+ President of the Medical Women’s Federation, the largest organisation representing medical women in the UK.
Chloe believes strongly in visible representation. She has spoken openly as a medical woman and an LGBTQ+ doctor. In 2022, Chloe wrote a piece for BMJ Leader discussing, for the first time openly, about her experiences of living with an invisible disability. Again, Chloe’s strong belief in visible representation made her a leader to disabled doctors and may others living with both visible and invisible disability.
Ove the past five years, Chloe has led the Faculty of Medicine and Dentistry (FMD) on Equality, Diversity and Inclusion (EDI) Lead as the EDI Lead and Athena SWAN Chair.
To mark her MBE, Chloe has written a lovely piece in the BMJ Leader detailing her experience with receiving this award. She has also kindly compiled a list of activism resources, available at the bottom of this page.
On receiving her MBE, Professor Orkin said:
“‘Serving the NHS for the past 26 years has been an enormous privilege, and it means a great deal that my contribution has been deemed valuable. By seeing someone like me receiving an MBE, I hope that others will see that they too can be recognised for their contributions to society. I look forward to serving my patients and colleagues for the rest of my career.”
Professor Sir Mark Caulfield, VP Health at Queen Mary University of London said:
“I am delighted to congratulate Chloe on receiving an MBE for her services to the NHS. Not only is Chloe an exceptional clinician and researcher, but she is also a role model and leader for many groups who have faced – and continue to face – challenge and discrimination across the world.
Chloe spearheaded change toward greater equality in our Faculty, overseeing our successful application for a Gold Athena SWAN award in medicine in 2023.
Congratulations, Chloe. This is hugely well deserved.”
Professor Yvonne Gilleece, Chair of the British HIV Association, said:
“As a past chair of the British HIV Association, Chloe has contributed so much to the development of new treatments for HIV and worked consistently to champion those facing stigma because of their HIV status, gender or ethnicity. We are delighted to see her recognised for her contribution to both medicine and society.”
Chloe has compiled a list of resources relating to her work on HIV, mpox, LGBT+ activism, and women in leadership.
Gender equity
Podcasts
Medical Women Podcast on leadership: The Medical Women Podcast: Episode 4: Stepping into leadership with Professor Chloe Orkin on Apple Podcasts
YANAF podcast: The Glass Slipper and Other Challenges for Women in Medicine – You Are Not a Frog
Research
Disability
Peer-reviewed publications on health equity
This article has been taken from Queen Mary University of London.

Tell us about your personal and professional motivation in regards to HIV research?
I am deeply interested in gender politics and am committed to improving the representation of women in clinical trials. It has always been clear to me that the importance of including women in HIV research needs to be underscored and addressed. My career has been and continues to be driven by the need to ensure that research reflects and benefits a diversity of individuals. A clear objective is transforming the landscape of HIV research to be truly representative and inclusive.
What challenges have you encountered in regards to women being adequately represented in clinical trials?
Women have always been under-represented in HIV treatment and that continues to this day. Research I presented only recently at the Conference on Retroviruses and Opportunistic Infections highlighted that in trials for long-acting injectable therapies, women were notably underrepresented with respect to the country proportion of women living with HIV.
How can such under-representation be addressed?
It requires a particular focus on those who have been historically marginalised. This means not just advocating for more inclusive research, but also designing studies that actively prioritise diverse participation. Effective strategies include intentional recruitment and inclusive protocol design. For instance, the ILANA study I led in the UK recruited over 50% women and people of colour, embedding an approach that countered sexism, racism, and ageism within its protocol.
What guidance would you offer to young researchers or clinicians who want to focus on improving healthcare inclusivity and efficacy for women with HIV?
Remember that patients are not hard to reach, it is our services that are hard to access. We need to tailor our services to what all of our patients need.
You were the global lead author for the FLAIR study which evaluated the first-ever long-acting injectable HIV therapy. Tell us about the key findings, and how they benefited the understanding and treatment of HIV in women.
Women made up around 20% of participants in the FLAIR study. When all the studies in long-acting injectable treatment with Cabotegravir and Rilpivirine (CAB+RPV) were pooled to establish a larger sample of women, there were no differences found between men and women, the treatment was equally effective. Such studies are crucial for developing treatment options that are accessible and effective. Representation is essential to ensure everyone can benefit equally from scientific advancement.
As a global medical leader for the U=U campaign, do you see this message particularly resonating with women living with HIV, or needing adaptation?
The Undetectable=Untransmittable message is powerful, yet there’s a need for nuanced communication. Some studies have shown that women have been slightly more sceptical of the message. It is also important to say that in breastfeeding the risk is negligible, not zero unlike all other circumstances. Again, tailoring the messaging to patients with specific realities is key.
Looking ahead, how do you envision HIV research and treatment evolving, particularly in relation to women’s health and inclusivity?
Women experience many inequities. Violence against women and girls is a huge factor in determining risk of acquiring HIV, and it is also something that women living with HIV experience. Our services need to be accessible and competent in identifying people affected by VAWG to signpost them to relevant services.
In terms of research, I hope that the global efforts to include women in trials will be successful. From a treatment point of view, long-acting PrEP has the potential to transform the ability of women to be in control of their HIV prevention options.
Advances in equitable research and healthcare will overall afford women greater autonomy and control over their health.
Finally, is it important that medical and academic circles also embrace representation, and where do you see your role within this?
Representation matters immensely. It’s vital to also embrace inclusion in terms of those who lead and conduct HIV research, as well as those who participate in it. As Billie Jean King said: you have to see it, to be it. As a visible LGBTQ+ advocate, and in roles I’ve held such as President of the Medical Women’s Federation, I try to make sure that younger people see me going about my business and register that there is a place for people like them in medicine and academia too. Diversity on both sides of research and clinical trials will only enrich our understanding and approach to healthcare long-term.
Article Credit: The National HIV Story Trust – https://www.nhst.org.uk/international-womens-day-professor-chloe-orkin-on-advocating-for-inclusion-in-hiv-research/
Dr Rageshri Dhairyawan was asked by The Lancet to write a review on the 3-part drama called ‘Breathtaking’ which highlighted the experience of the Covid-19 pandemic on frontline medical staff and how they desperately worked hard to save lives. For the full article, please follow the link here.

The awards ceremony, held on 25 May 2023 at the Law Society, brought together nominators nominees and their team members to recognise exceptional work and expertise delivered by teams and individuals from across the university in eight categories. The Research and Innovation awards is to be held annually to recognise the exceptional research conducted at Queen Mary.
The SHARE collaborative found success during this ceremony by securing two awards for innovative research conducted amongst the team. The categories won were the following:
For further information on the remaining categories and other awards won, please follow the link here.

Team SHARE hosted their first virtual symposium on 5th May 2021, chaired by Ms Sheila Gupta, Vice-Principal (People, Culture and Inclusion) Queen Mary University of London.
The symposium outlined the purpose of SHARE and each research theme. Talks were presented by Prof Chloe Orkin, Prof Jane Anderson, Dr Vanessa Apea, Dr John Thornhill, Dr Rageshri Dhairyawan and Ms Angelina Namiba (HIV Community Representative).
Watch the full symposium below.
Fast-Track Cities London and the Worshipful Society of Apothecaries hosted a joint webinar on Wednesday 23 June to mark 40 years since the first description of AIDS and explore the progress that has been made in treatment for HIV. The focus was on people and their experiences of AIDS and HIV.
We heard from people with HIV, doctors and nurses about treatment then and how it has evolved, what has been achieved so far and how looking after people has changed from a patient and clinical perspective. The panel also identified remaining challenges and actions needed so people get the best health outcomes, and what needs to happen next to reach London’s 2030 goal of “Getting to Zero”.
Speakers and panellists were:
Fast-Track Cities London is part of a global movement of cities to end HIV by 2030. The Mayor of London joined NHS England, London Councils and Public Health England to sign up to this commitment in 2018. It has brought together everyone working to end HIV with people living with HIV, the NHS, London’s Councils, doctors, nurses, public health experts and academics. It is the only place that brings everyone working in the HIV sector in London together. The roadmap to zero is a jointly designed action plan that shows the steps London will take to get to zero new cases of HIV, zero preventable deaths and zero stigma. Find out more here: www.fasttrackcities.london
The Worshipful Society of Apothecaries is the City of London Livery Company that represents doctors and pharmacists. The Society hosts the Diploma in HIV Medicine, which sets the professional standards for doctors involved in the care of people living with HIV. The Society has a particular interest in the history of medicine and pharmacy with its faculty of the History and Philosophy of Medicine. The Society is also a founder member of the Health Liveries group. Visit www.apothecaries.org to find out more.
On Tuesday 22 June 2021, National AIDS Trust hosted this online conversation exploring HIV and migration and the barriers faced by people born abroad living with HIV in the UK, chaired by Deborah Gold (Chief Executive at National AIDS Trust). Dr Rageshri Dhairyawan served as an advisor for this project and panellist at the virtual event.
Panellists are:
62% of all new HIV diagnoses in the UK in 2019 were among people born abroad. Half of these acquired HIV since moving to the UK. Despite this, there is currently no shared understanding of the policies and interventions needed to support people born abroad from acquiring HIV in the UK, and overcome barriers to testing and treatment for those living with HIV.
To end new transmissions of HIV by 2030, an accepted national commitment, we must make progress for all population groups, including those board abroad. National AIDS Trust wanted to understand the barriers they face when accessing HIV testing, treatment and care.
This event launched our latest report – HIV and migration, and shares our research findings and the recommendations we have made to improve the health outcomes and quality of life of those born abroad and living with, or at higher risk of, HIV.
The full report can be found here: www.nat.org.uk/publication/hiv-and-migration
The UK has passed the terrible milestone of 100,000 deaths with COVID-19. These losses have not been evenly spread throughout different communities. A disproportionate number of both severe cases and deaths have been among those from Black, Asian, and minority ethnic (BAME) backgrounds.
In England, analyses of data from the Office of National Statistics and National Health Service has revealed 2.5-fold to 4.3-fold greater COVID-19 mortality rates across a range of Black and South Asian ethnic groups compared with white groups.
As doctors working on the frontline of COVID-19 care, we wanted to understand the driving factors behind the differences in outcomes between ethnic groups within our community of East London, which was at the epicentre of the pandemic during the first wave. Our study included all of the 1,737 COVID-19 patients who were admitted to the five hospitals within Barts Health NHS Trust between January 1 and May 13 2020.
In contrast to many previous studies examining ethnicity and COVID-19 outcomes, we were also able to address how a range of factors including social and economic background, previous underlying conditions, lifestyle and demographic factors contributed to how patients fared.
In our sample, patients from Black, Asian and other minority ethnic backgrounds were significantly younger and less frail when they were admitted to hospital than white patients.
Black patients were 30% and Asian patients 49% more likely to die within 30 days of hospital admission compared to patients from white backgrounds of a similar age and baseline health. Black patients were also 80% and Asian patients 54% more likely to be admitted to intensive care and need invasive mechanical ventilation.
This graph shows predicted survival of Asian, Black and white ethnic groups to 30 days following hospital admission for a male patient aged 65. Probability of survival reduces as time passes but there are significant differences between Asian and Black compared to white patients, and these differences also increase over time.
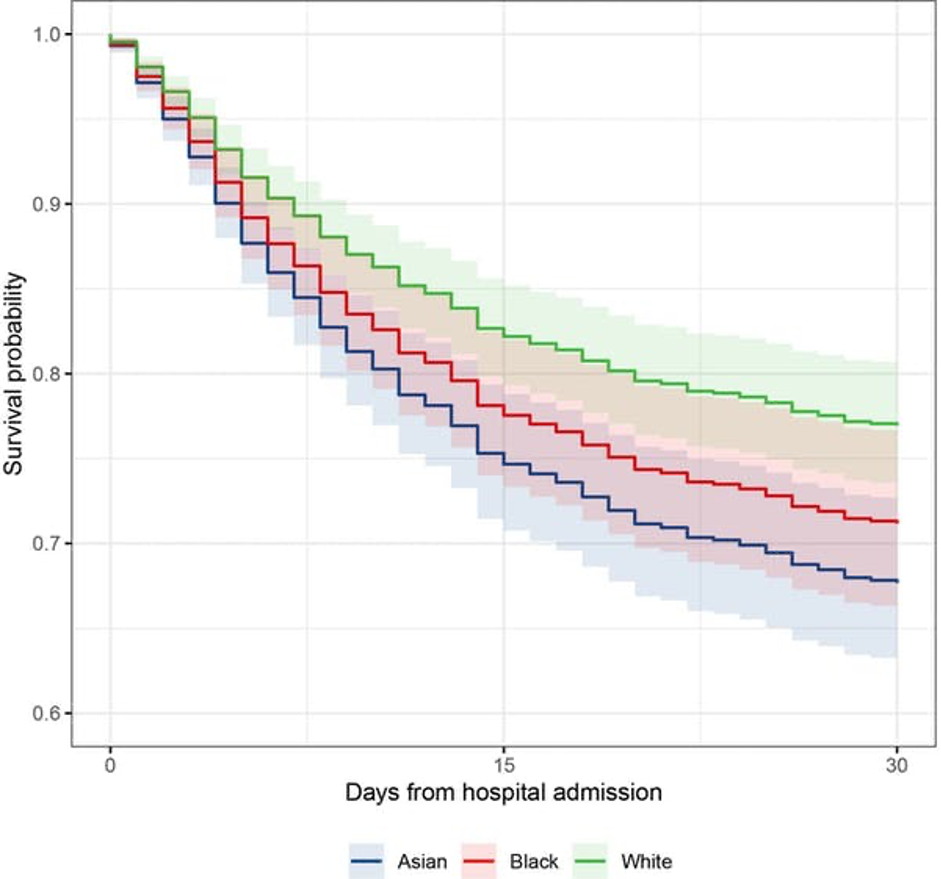
When we accounted for the role of underlying health conditions, lifestyle, and demographic factors, the risk of death in Black and Asian populations did not drop to the same rates as white patients.
In our cohort, all ethnic groups experienced high levels of deprivation, however, worse deprivation was not associated with higher likelihood of mortality. This suggests ethnicity may affect outcomes independent of purely geographical and socioeconomic factors.
The risk factors associated with worse underlying health status are likely to be linked with wider social factors such as poor living conditions, being employed as a key worker and even language barriers that may get in the way of people adopting preventative measures to avoid getting sick. Structural racism also plays a role in generating and reinforcing inequities and must be acknowledged and addressed.
Although our study had a large number of patients, it was not possible to assess a more detailed ethnicity breakdown and so may not reflect the vast diversity that exists within ethnic categories (such as Bangladeshi, Pakistani, black African or black Caribbean). Future studies should focus on exposing specific inequalities that may exist between these sub-ethnic categories.
Similarly, we need bigger sample sizes to contextualise a number of potential factors including household composition, environmental concerns and occupation.
Although COVID-19 has placed ethnic inequalities in health outcomes in sharp focus, these differences have been widely documented for decades.
In another study, we are working directly with local residents in East London to understand their experiences both before and during the pandemic, so we can begin to find solutions together.
As the impact of COVID-19 persists, we continue to see significant numbers of Black, Asian, and minority ethnic patients admitted to our hospitals. The aftermath of this is yet to seen in its entirety as, in addition to the high rates of premature death suffered among these population groups, these frequently working-age patients will often leave hospital with long-term chronic health conditions, returning home with a greatly reduced quality of life.
We must respond now to the ethnic disparities that have been highlighted by the COVID-19 pandemic if we want to prevent them being inflicted on future generations.
Dr Yize Wan is a Clinical Lecturer in Intensive Care Medicine at Queen Mary University of London.
Dr Vanessa Apea is a Consultant Physician in Sexual Health and HIV Medicine at Queen Mary University of London.
News items relating to this story:
Evening Standard